Adding savolitinib to osimertinib beneficial for certain pretreated lung cancer patients
ATLANTA -- Adding the investigational MET inhibitor savolitinib to the EGFR inhibitor osimertinib (Tagrisso) yielded clinical responses in patients who had EGFR-mutant non-small cell lung cancer (NSCLC) that had developed resistance to prior EGFR-targeted therapies through MET-gene amplification, according to interim results from two expansion cohorts of the phase Ib clinical trial TATTON, presented at the AACR Annual Meeting 2019, March 29-April 3.

Savolitinib
"To date, targeted therapy for lung cancer patients with EGFR mutations has consisted solely of monotherapy with various EGFR tyrosine kinase inhibitors (TKIs), though we have known for more than 10 years that a proportion of resistance to EGFR TKIs results from activation of the MET bypass pathway," said Lecia V. Sequist, MD, MPH, a thoracic medical oncologist and director of the Center for Innovation in Early Cancer Detection at Massachusetts General Hospital Cancer Center.
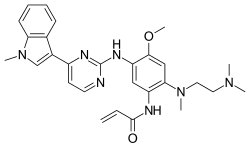
Osimertinib
Prior research has shown that MET amplification is a bypass pathway observed in about 5 to 10 percent of patients whose disease has progressed after treatment with first- or second-generation EGFR TKIs and in about 25 percent of those whose disease has progressed after treatment with third-generation EGFR TKIs, Sequist explained.
Prior clinical trials of combinations of EGFR- and MET-targeted therapeutics have not been successful, partly due to the drug combinations studied, and largely because patients were not chosen based on appropriate biomarkers, Sequist said. "In the TATTON trial, newer TKIs that have increased specificity for EGFR and MET are used, and patients with EGFR-mutant NSCLC are required to have documented MET-driven resistance," she added.
Interim results from two distinct expansion cohorts are presented here. In the first cohort, a combination of osimertinib and savolitinib was tested in patients with EGFR-mutant lung cancer with acquired resistance driven by MET amplification after treatment with a first- or second-generation EGFR TKI; these patients' tumors were also negative for T790M mutation. In the second cohort, the same combination was tested in patients with EGFR-mutant lung cancer with acquired resistance driven by MET amplification after treatment with osimertinib or another experimental third-generation EGFR TKI.
"Data from the TATTON trial demonstrate for the first time the benefit of adding a MET inhibitor to an EGFR inhibitor in patients with EGFR-mutant NSCLC and with MET-driven acquired resistance," Sequist said. "The study has shown efficacy of combination targeted therapy in a patient population for whom chemotherapy is the current primary treatment option.
"This finding illustrates the value of careful patient selection in studies of targeted therapies," Sequist said, adding, "These clinically meaningful responses also demonstrate that as different heterogeneous resistance clones come up, they can in turn be brought under control by tailoring therapy."
In the cohort of 46 patients who had received prior first- or second-generation EGFR TKI, treatment with osimertinib plus savolitinib yielded an objective response rate (ORR) of 52 percent, with 24 partial responses. The median duration of response (DOR) was 7.1 months.
In the cohort of 48 patients who had received prior third-generation EGFR TKI, treatment with osimertinib plus savolitinib yielded an ORR of 28 percent, with 12 partial responses. The median DOR was 9.7 months.
"Overall the regimen was tolerable, though there was added toxicity with the combination of osimertinib and savolitinib compared to osimertinib given alone, and we saw that some patients discontinued treatment due to toxicity," Sequist said. The most frequent adverse events were nausea, diarrhea, and lowered numbers of leukocytes and platelets.
One patient, who had brain metastases, died from kidney failure a few days after starting the combination treatment. The treating investigator considered that this serious adverse event was difficult to evaluate with respect to relation to the study drugs, Sequist said. "Our understanding of the adverse event profile of the osimertinib-savolitinib combination, and how to manage the adverse events, is improving," she added.
Since the initiation of the TATTON trial, osimertinib was approved for treatment in first-line setting for patients with EGFR-mutant NSCLC. Because of this, only a subset of patients in the trial had received prior first-line osimertinib and had developed MET-driven resistance. "The newly opened phase II SAVANNAH study will further explore the combination of osimertinib plus savolitinib in patients whose disease has progressed on osimertinib and is MET-positive," Sequist said.
These are early-phase trials and the findings need confirmation in larger trials, Sequist noted.
###
The TATTON trial was funded by AstraZeneca. Sequis
PUBLIC RELEASE:
https://eurekalert.org