2 common psychiatric drugs may slow progression of Alzheimer’s, study shows

Researchers from the University of Colorado School of Medicine analyzed drugs that could block the effect of the apolipoprotein E4 protein (APOE4), which is a risk factor gene for Alzheimer’s.
While screening different medications that could have this effect, they came across two commonly prescribed psychiatric medications: imipramine and olanzapine.
The researchers observed that the use of these medications in patients with Alzheimer’s disease was associated with better clinical diagnoses and improved cognition, compared to other antidepressant and antipsychotic drugs.
Alzheimer’s disease is a form of dementia that initially causes memory loss and cognitive decline. The disease may eventually progress to the point where someone loses all cognitive function.
Imipramine
According to a June 2022 study published in Alzheimer’s Research & Therapy, there are two drugs with prior Food and Drug Administration (FDA) approval that may be beneficial for people with Alzheimer’s disease. The drugs, imipramine and olanzapine, are already used to treat psychiatric conditions.
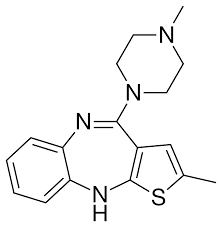
Olanzapine
A research team from the University of Colorado Anschutz Medical Campus in Aurora led the study.
Alzheimer’s disease background
There are multiple forms of dementia, including mixed dementia, Lewy body dementia, and Alzheimer’s disease. According to the Alzheimer’s Association, Alzheimer’s is the most common form of dementia and accounts for 60 to 80% of dementia cases.
While Alzheimer’s can affect younger people, including people in their 30s and 40s, this is not common. Alzheimer’s typically occurs in people ages 65 and older.
The National Institute on Aging (NIA) includes some of the following signs and symptoms of Alzheimer’s:
- memory loss
- confusion
- mood changes
- poor judgment
- difficulty with language
- troubling carrying out tasks with multiple steps
- aggression
Scientists do not fully understand what causes Alzheimer’s, but some think that a combination of genetic and environmental factors may lead to developing the disease.
There is no cure for Alzheimer’s, but healthcare providers may prescribe medications such as donepezil or galantamine to decrease symptoms. And, in some cases, providers may prescribe psychiatric drugs to patients with Alzheimer’s when other treatments haven’t adequately helped with aggression, anxiety, and depression symptoms.
Psychiatric drugs for Alzheimer’s
The research team at the University of Colorado School of Medicine was primarily interested in finding medications that could block APOE4, which they hypothesize could reduce someone’s chance of developing Alzheimer’s.
While looking into drugs that could have this effect, the team noticed that two of the medications are commonly prescribed for psychiatric conditions. The medications were imipramine and olanzapine; imipramine is a tricyclic antidepressant, and olanzapine is an antipsychotic.
“We then looked into the huge National Alzheimer’s Coordinating Center database and asked what happened when someone was prescribed these drugs for normal indications but happened to be Alzheimer’s patients,” said Huntington Potter, PhD, professor of neurology and director of the CU Alzheimer’s and Cognition Center at the University of Colorado Anschutz Medical Center.
Potter and his team observed that Alzheimer’s patients who took imipramine and olanzapine, compared to other antidepressant and antipsychotic drugs, saw improvements in cognition that could help reverse the progression of the disease.
“The people who received these drugs developed better cognition and actually improved in their clinical diagnosis,” Potter said. “Compared to those who did not take these drugs, they reverted from Alzheimer’s disease to mild cognitive impairment or from mild cognitive impairment to normal.”
The researchers next looked at biological sex to see whether there is a difference in how men and women respond to the cumulative effects of taking imipramine. Their calculations showed that men between the ages of 66.5 and 88.5 years saw the most benefit.
The authors wrote that taking imipramine for a long period of time “increased the incidence of reversion to a better clinical diagnosis for men.” While women also saw an improvement, the authors note that it was not “statistically significant” compared to men.
What experts have to say
Dr. Tom MacLaren, a consultant psychiatrist at Re:Cognition Health, spoke with Medical News Today about the study findings.
“This could be another important step in finding new treatments for dementia,” Dr. MacLaren commented.
Dr. MacLaren acknowledges that more research is needed and noted a positive for using these two medications in patients with Alzheimer’s.
“The advantage is that both imipramine and olanzapine have been around for a very long time, and so we know they are safe,” Dr. MacLaren said.
Dr. Clifford Segil, a neurologist at Providence Saint John’s Health Center in Santa Monica, CA, told MNT he had some reservations about the study findings.
“Most lab research in Alzheimer’s dementia has not resulted in real-world changes or new clinically proven beneficial medications for my patients with memory loss. What happens on a calculator does not translate to what is going to happen in my office, more often than not, with Alzheimer’s dementia,” Dr. Segil said.
“In clinical practice, these medications should remain reasonable to use for patients with depression and as antipsychotic medication, but there should be no hope that they will improve cognition in addition to depression or psychosis.”
Study limitations
The study authors noted that while the dataset they reviewed was the largest available, it was still relatively small compared to what they would review for a clinical trial.
Additionally, the authors concede that it is “possible that a clinician’s prescription of a certain antidepressant or antipsychotic may have been determined by patient comorbidities (e.g., diabetes, hypertension, etc.) that could have had independent effects on cognition.”
The authors plan to continue studying these medications and plan to conduct a trial testing imipramine on mice.
July 7, 2022



